Position Statement: On NYS Attorney General’s Report on COVID-19 and Nursing Home Mortality: Poor Staffing Levels Contributed to High Death Toll
On January 28, the NYS Attorney General issued a report on the impact of COVID-19 on the state’s nursing home residents.
The report found that at least 6,645 nursing home residents died of COVID between March and November, accounting for about 25% of all deaths statewide during that time period.
The AG’s report demonstrates that the death toll among nursing home residents was undercounted by 50%, because the State DOH did not include residents who died after being taken to hospitals or other sites of care in the measure of nursing home resident deaths.
The initial reaction to the AG’s report has focused on whether the state DOH tried to hide the true extent of the death toll in nursing homes.
The more important and damning finding in the AG’s report is that high mortality rates in nursing homes are largely attributable to a chronic pattern of inadequate staffing levels in nursing homes that was worsened by the onset of the pandemic. Current state law gives operators wide latitude to determine the number of RNs, LPNs and Aides they use to provide resident care. This has resulted extreme variations in the level of staffing and patient care from facility to facility. The arrival of COVID exposed these vulnerabilities and made them worse.
The central finding and core recommendation of the AG’s report is that poor staffing was a major factor in the high death toll in nursing homes and that New York must enact enforceable, minimum staffing standards or hours of care per resident. If we had required nursing home operators to provide mandatory levels of RN, LPN and Aide staffing, thousands of lives would have been saved.
1. Direct correlation of poor staffing and higher mortality rates in nursing homes
The AG’s report shows a direct correlation between poor staffing and higher death rates among nursing home residents.
Using CMS “nursing home compare” data and rankings, the AG report found that the nursing homes with the lowest staffing ratings had mortality rates that were 44% higher than those with the highest rating.
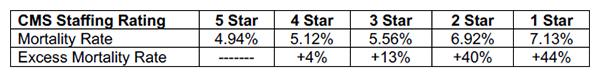
If state law had required all nursing homes to meet the staffing levels of “5 Star” CMS-rated facilities, the 6,645 deaths in nursing homes would have been reduced to 5,094 - 23.34% fewer deaths or 1,551 lives saved.
When the authors of the AG’s report weighted the mortality data by staffing levels and geography, the difference between the best staffed and lower ranked facilities was even more pronounced:
- Weighted mortality rates for residents of facilities receiving the top “5 Star” staffing rating were less than half the mortality rates of the rest of the facilities;
- If all facilities were staffed at the “5 Star” standard, 3,300 fewer nursing home residents would have lost their lives between March and November.
2. Poor staffing and ineffective infection control measures increased risks of resident harm
Many nursing homes failed to prepare and implement infection control protocols to protect residents from exposure to COVID.
The AG’s report identifies the following infection control factors that contributed to high mortality rates: failure to isolate patients with COVID; improper or inadequate sterilization of equipment and surfaces; continued communal dining and other less labor intense patient care practices; failure to screen or test direct care staff for COVID; pressuring or mandating exposed or sick staff to report to work; failure to train direct care staff on proper infection control measures; and failure to provide personal protective equipment (PPE) to protect staff from COVID exposure. Understaffed facilities did not have the ability to devote extra time to implementing heightened COVID infection control measures.
The proper implementation of infection control measures is directly or indirectly attributed by the report to a lack of direct care staff, particularly of RNs, who are responsible for creating and implementing patient care plans. Infection control in the closed space of a nursing home is a labor intensive process. Insufficient staffing undermined efforts to protect residents and contributed to the high death.
3. The prevalence of for-profit operators contributed to poor staffing and infection control
More than 65% of the nursing homes in New York are operated by for-profit owners, 31% by non-profit companies, and 5% by the government. The AG’s report notes that the drive to maximize revenues and enrich the operators of these for-profit facilities played a key role in the high mortality of residents.
The report notes that the lowest staffing levels and the highest mortality rates were concentrated in the for-profit nursing home group, which comprised more than 81% of the worst staffed “1 Star” and “2 Star” facilities. Conversely, non-profit and government facilities made up 88% of the top ranked “5 Star” staffed nursing homes.
According to CMS data, for-profit operators received 79% of verified citations for safety violations. Government-run nursing homes provided a total average of 4.40 hours of direct nursing care per patient day (HPPD) and non-profits provided 4.14 hours. For-profits, in comparison, provided only 3.45 hours per day – 20% lower than non-profits and 30% lower than government-run facilities.
4. Safe staffing also saves lives in hospitals
The AG’s report on nursing homes does not address the impact of staffing levels in hospitals and COVID mortality rates. There is, however, ample evidence that lower staffing in hospitals also contributed to COVID higher mortality, including of nursing home residents who were transferred to hospitals.
Researchers at the University of Pennsylvania found that understaffing had adverse consequences on nurses and on patient care, and that understaffed hospitals pose a public health risk. (http://bit.ly/BMJStaffing). The New York Times reported that the better staffed and resourced flag-ship hospitals of large NY City area systems had lower mortality rates than their less resourced and understaffed hospitals in the outer boroughs. The Wall Street Journal recently reported on the impact on mortality rates in hospitals relying on “lean” staffing plans that rely on supplemental temporary staff to respond to surges in demand. he weakness of these cost-cutting staffing models is a central finding of the AG’s report, and it applies equally to our hospital system. All nursing home residents and hospital patients should be protected by minimum staffing standards that apply to all facilities equally.
5. Enact mandatory minimum staffing guidelines in NY nursing homes and hospitals
One of the core recommendations of the AG’s report is to enact minimum caregiver to resident staffing guidelines in our nursing homes.
The legislature should immediately enact the “Safe Staffing for Quality Care Act” (A108/S1168). This legislation will require minimum RN, LPN and Aide staffing hours for nursing home residents and minimum staffing standards in our hospitals. Passing safe staffing legislation will save lives and address the devastating shortcomings in our health care system identified by the Attorney General.